The Promise of Bedside Brain Imaging in Babies
Image source here
When a baby is first born, our initial thoughts tend to be of the excitement, happiness, and relief following the delivery. Sadly, this is not always the case. In the neonatal intensive care unit (NICU), there is often an air of trepidation and tension. Here, babies who were born preterm can be found in cots surrounded by beeping machines and busy healthcare workers providing round-the-clock care to keep them alive. These preterm infants demonstrate remarkable strength and resilience, fighting to overcome immense challenges from the moment they take their first breath.
Babies are classed as “preterm” when they are born before 37 weeks of gestation, compared to the full-term pregnancy of around 40 weeks. It is estimated that around 13 million babies are born early every year (World Health Organization), and thanks to advances in medicine these babies have a much greater chance of survival now than they would have in the past. Still, preterm babies face many health challenges with one major concern being their brain development.
Premature babies are at a particularly high risk for a specific type of brain bleed, also known as a hemorrhage. This is the most common complication for brain development in this group and in severe cases can be life-threatening. This type of brain bleed is a result of the infants’ blood vessels not being fully developed, which makes them susceptible to rupture and bleeding. Hemorrhages like this tend to occur in the first few days or weeks of life, when the brain is especially vulnerable. In preterm infants, this often affects cavities in the brain known as the ventricles. Increased blood in the ventricles can lead to swelling of the head, seizures, and clinical decline, which means preterm babies must be carefully monitored.
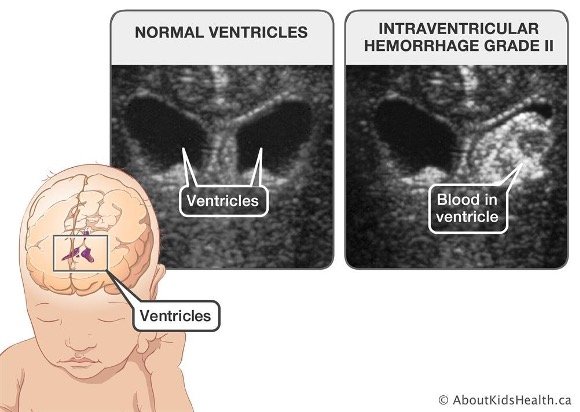
Figure 1: Example of ventricular hemorrhage in a preterm infant detected by 2-dimensional (2D) ultrasound. Source here.
Currently, hemorrhages in the ventricles are diagnosed using a head ultrasound and given a grade from I – IV, depending on severity. Figure 1 shows an example of a hemorrhage affecting the ventricles in a preterm infant. This demonstrates how blood in the ventricles can be seen in the image from the ultrasound.
In a recent publication, a team of researchers from Western University, London Health Sciences Centre, and the Children’s Health Research Institute explored brain imaging methods suitable for bedside use in the NICU for monitoring hemorrhages. The research team set out to explore additional tools for monitoring hemorrhage using optical neuroimaging and 3-dimensional (3D) ultrasound. These techniques are useful as they allow doctors and researchers to get a better idea of what is happening in the brain.
Functional near-infrared spectroscopy (fNIRS) is a brain imaging technique that relies on light to measure the blood dynamics, a marker of brain activity. This is based on the knowledge that when a brain region is more active, it requires more oxygen, causing blood flow in that area to increase. To study the blood flow, small light sources are attached to a cap which fits snugly on the head and light is shone onto the scalp. From there, light passes through the scalp, skull and fluids into brain tissue. Based on how much light is absorbed by these tissues, it is possible to determine how much oxygen a brain region is using at a given time.
fNIRS is comparable to the common imaging modality known as functional magnetic resonance imaging (MRI), which provides us with detailed images of brain structure and can be used to measure blood flow. MRI machines are large and immobile, and because they rely on a huge magnet they are generally kept in shielded rooms. However, fNIRS has the great advantage of being able to be used at bedside in the NICU. This minimizes any need to transport preterm babies to different parts of the hospital, a journey which can be dangerous and should be avoided whenever possible. To complement the fNIRS measures, the team also used 3D ultrasound, which adds extra dimension and, therefore, depth, to the imaging achieved using traditional ultrasound. This results in more detailed visualization of the brain and has shown promise in identifying which preterm babies may require surgical intervention. In turn, surgical intervention may help to minimize long-term damage to the brain and improve health outcomes.
A total of 30 babies were enrolled in the study, all of whom were born at 32 weeks or earlier. Each infant underwent the standard 2D ultrasound within one week following birth and again at one month. Seven of the enrolled babies underwent surgical intervention, with necessity for this procedure being determined by the paediatric neurosurgeon. All of the measures, including 3D ultrasound and fNIRS, were recorded with infants lying in the incubator cot in the NICU. Each of the patients included in the study underwent recording for fNIRS and 3D ultrasound on multiple occasions.
The 3D reconstructed image was used to determine the size of the ventricles in the preterm infants, which are often enlarged following brain bleeds. It is important to be able to assess the ventricle size, as enlarged ventricles, if left untreated, can severely impact brain development. The fNIRS recordings of brain activity were used to explore functional connectivity between regions. Connectivity is a useful measure of brain health and function, as it indicates how well brain regions are communicating and relaying information.
Following analyses, the researchers were able to conclude that there was a relationship between the ventricle size and functional connectivity. Specifically, they found that larger ventricles were associated with decreased functional connectivity. The authors conclude that this is indicative of structural changes in the brain which may impact development and the ability of regions to communicate with one another. This provides support for the use of extra monitoring tools in the NICU, especially if it will assist in identifying the best time for successful intervention.
Used together, 3D ultrasound and fNIRS offer a sophisticated, non-invasive, and non-disruptive way of assessing brain structure and function in preterm babies. Ultimately, the integration of brain imaging in the NICU represents significant advances in the medical field and is likely to help in identifying early interventions and improving outcomes for preterm infants.
Original article:
Kebaya, L.M.N., Stubbs, K., Lo, M., Al-Saoud, S., Karat, B., St Lawrence, K., de Ribaupierre, S. & Duerden, E.G. (2023) Three-dimensional cranial ultrasound and functional near-infrared spectroscopy for bedside monitoring of intraventricular hemorrhage in preterm neonates. Sci Rep 13, 3730.
https://doi.org/10.1038/s41598-023-30743-4
Other references:
https://www.who.int/en/news-room/fact-sheets/detail/preterm-birth